MICROBIAL INFECTIONS OF HUMANS(HUMAN MICROBIOLOGY CONTD..)
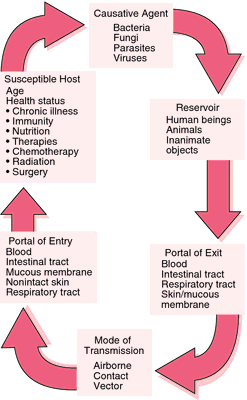
MODE OF TRANSMISSION:
The ability to reproduce will be the ultimate driving force for all organisms. For bacteria that infect
humans there are several routes that can be employed to infect new hosts. The various means by which a
micro-organism may be transmitted from the source to the new host.Note that some organisms can be spread by more than one mode of transmission. Measles virus is likely to be spread by airborne and direct
contact. The number of times people touch their faces with their hands is enough to almost guarantee
that virus in the nose or saliva will be transferred to the hands. You will notice other flaws in the
scheme. The table distinguishes between sexually transmitted infections and those obtained by direct
contact. It could be argued that they are the same mode of transmission. The example of dermatophytes
as directly transferred infections also needs qualifying. In the latter cases the fungi are often transmitted
through shared, inanimate objects like towels or combs. This is not direct transmission in the strictest
sense. Perhaps ‘indirect transmission’ is a more appropriate term.
Two important terms are vertical transmission and horizontal transmission. Rather than referring to
positions of the host when they came into contact with the infectious agent (!) they are used to
distinguish between infections transferred from mother to child (vertical) and those acquired from other
sources (which in this context means predominantly people) and are called horizontal. Two of the most
important examples of vertical transmission are rubella virus and Treponema pallidum(syphilis). Such
infections of the foetus can have serious developmental consequences. Congenital rubella, for example,
may lead to microcephaly (small head), impaired vision and impaired intellectual development.
The significance of vertical or horizontal transmission for the microbe lies in the number of people that
can be infected. With vertical transmission only one new host is infected and that is the child (or
children). With horizontal transmission there is the opportunity to infect significantly greater numbers of
people. It follows then that if one person is able to infect five others, these five will then infect 25 and so
on.
The exact point at which infections of the newborn baby stop being vertical transmission and become
horizontal is debatable. Certainly vertical transmission can be subdivided into:
• germline transmission (spread of virus integrated within the genome),
• prenatal transmission (infection of the foetus in the uterus),
• perinatal transmission (infection during birth),
• postnatal transmission (infection following birth).
Strictly, only infections of the foetus in utero are vertically transmitted. Perinatal infections (those
acquired by the baby in the vaginal tract during the process of delivery) and postnatal infections (e.g.
acquired via breast milk) are horizontally transmitted.
Vector-borne infections are those that are transferred by a vehicle/carrier, which are insects. The term
vector is (most usefully) restricted to living animals such as lice, fleas or mosquitoes. Combs and
hairbrushes are thus not usually called vectors, but fomites. The transfer of dermatophytes via
hairbrushes is best described as ‘direct transfer’. Vectors serve to transmit organisms from the
bloodstream of infected patients to new susceptibles. The organisms (notably arboviruses: arthropod borne viruses and protozoan parasites such as malaria) are not designed to withstand any time outside of
a host. The transfer of the organism is dependent on the distances the vector can travel in its lifetime. A
wide range of insects transmit infectious microbes.
ZOONOSES:
The ability to reproduce will be the ultimate driving force for all organisms. For bacteria that infect
humans there are several routes that can be employed to infect new hosts. The various means by which a
micro-organism may be transmitted from the source to the new host.Note that some organisms can be spread by more than one mode of transmission. Measles virus is likely to be spread by airborne and direct
contact. The number of times people touch their faces with their hands is enough to almost guarantee
that virus in the nose or saliva will be transferred to the hands. You will notice other flaws in the
scheme. The table distinguishes between sexually transmitted infections and those obtained by direct
contact. It could be argued that they are the same mode of transmission. The example of dermatophytes
as directly transferred infections also needs qualifying. In the latter cases the fungi are often transmitted
through shared, inanimate objects like towels or combs. This is not direct transmission in the strictest
sense. Perhaps ‘indirect transmission’ is a more appropriate term.
Two important terms are vertical transmission and horizontal transmission. Rather than referring to
positions of the host when they came into contact with the infectious agent (!) they are used to
distinguish between infections transferred from mother to child (vertical) and those acquired from other
sources (which in this context means predominantly people) and are called horizontal. Two of the most
important examples of vertical transmission are rubella virus and Treponema pallidum(syphilis). Such
infections of the foetus can have serious developmental consequences. Congenital rubella, for example,
may lead to microcephaly (small head), impaired vision and impaired intellectual development.
The significance of vertical or horizontal transmission for the microbe lies in the number of people that
can be infected. With vertical transmission only one new host is infected and that is the child (or
children). With horizontal transmission there is the opportunity to infect significantly greater numbers of
people. It follows then that if one person is able to infect five others, these five will then infect 25 and so
on.
The exact point at which infections of the newborn baby stop being vertical transmission and become
horizontal is debatable. Certainly vertical transmission can be subdivided into:
• germline transmission (spread of virus integrated within the genome),
• prenatal transmission (infection of the foetus in the uterus),
• perinatal transmission (infection during birth),
• postnatal transmission (infection following birth).
Strictly, only infections of the foetus in utero are vertically transmitted. Perinatal infections (those
acquired by the baby in the vaginal tract during the process of delivery) and postnatal infections (e.g.
acquired via breast milk) are horizontally transmitted.
Vector-borne infections are those that are transferred by a vehicle/carrier, which are insects. The term
vector is (most usefully) restricted to living animals such as lice, fleas or mosquitoes. Combs and
hairbrushes are thus not usually called vectors, but fomites. The transfer of dermatophytes via
hairbrushes is best described as ‘direct transfer’. Vectors serve to transmit organisms from the
bloodstream of infected patients to new susceptibles. The organisms (notably arboviruses: arthropod borne viruses and protozoan parasites such as malaria) are not designed to withstand any time outside of
a host. The transfer of the organism is dependent on the distances the vector can travel in its lifetime. A
wide range of insects transmit infectious microbes.
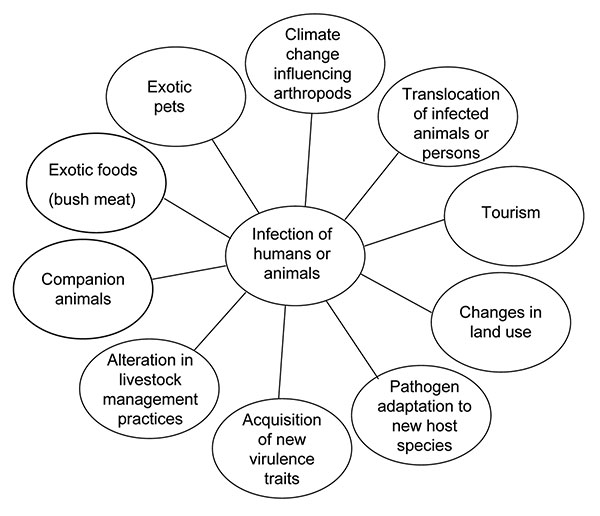
ZOONOSES:
Zoonoses are infections that can be transmitted between vertebrate animals and humans (singular:
zoonosis). The natural host is the animal. Often a human infection represents a dead-end in terms of
perpetuating the spread of the organism because we are unlikely to pass the organism to another animal.
Having mentioned malaria as an arthropod-borne infection, one should note that malaria in man is not a
zoonosis. There are numerous (hundreds) of animals that are infected with different Plasmodium spp.
but the plasmodia that commonly cause disease in humans appear to have evolved so that humans are
the ‘natural’ hosts, thereby disqualifying themselves as zoonoses.
SOURCES OF ZOONOSES
Zoonoses have arisen mostly through the need of humans to collect food. Humans have
been able to domesticate animals both as livestock (cows, pigs, etc.) and as helpers
(sheepdogs) as well as deforesting areas for crops. These activities bring man into close
contact with the micro-organisms that infect the animals. Tuberculosis, anthrax and
brucellosis are caught directly from farmed animals. Others arise from those animals we
encounter whilst disturbing them in their natural habitats (yellow fever, Lyme disease,
Ebola virus). Not that zoonoses are only caught by venturing into dark jungles! Pets are a
common source of various microbes that can cause human disease, especially fungal
dermatophyte infections. More important in terms of national public health is food
poisoning. Increasing in incidence in the Western world, Salmonella enteritidis and
Campylobacter jejuni are the leading causes of food poisoning in developed countries.
Mostly as a result of battery farming, both organisms are frequently isolated from uncooked
chickens but inadequate precautions in food hygiene fails to reduce their numbers to below
the infectious dose necessary to induce food poisoning. Despite being a preventable
infection, food poisoning is a national public health concern and burden in lost manpower
to industry.
The transmission from the animal to humans (and it is only this direction that concerns us here!) can be
separated further, depending on the natural life cycle of the micro-organism in question.
1. Direct transmission (direct zoonosis): transmission occurs via direct contact from the original
animal (e.g. rabies transferred through the saliva of the dog). The microbe does not undergo any
developmental change between the two hosts (rabies, brucellosis).
2. The micro-organism has an intermediate (or secondary) host in its complete life-cycle and humans
can only become infected with the infective stage of the organism at the appropriate stage of the
micro-organism’s life cycle (plague, schistosomiasis).
3. The organism infects humans having spent a period in a non-living site. The organism may develop
into the infective form (e.g. hookworm larvae hatch from the eggs present in the soil contaminated
with faeces. When someone sits on the soil, the larvae penetrate the skin). Other infections are
caught from the non-living site without any developmental change in the organism (e.g.
cryptococcal infections, other invasive mycoses, leptospirosis).
Staphylococcus aureus food poisoning is due to the consumption of preformed toxin in the
food. The enterotoxin triggers vomiting which occurs quickly (5–8 hours after ingestion of the
toxin). Salmonella food poisoning, however, is due to ingestion of large numbers of
organisms, at least 106/gm. The diarrhoea results from the multiplication in the small intestine
and this takes 18 hours before the patient develops symptoms. This highlights the inaccuracy
of the term ‘food poisoning’ because the poisoning implies chemical- or drug-induced
toxicity.
By considering the natural reservoir of the organism, one is able to plan what precautions can be taken to
prevent a recurrent infection or an outbreak. Knowing the route of transmission offers the possibility of
breaking the flow of organisms. A consideration of food poisoning organisms illustrates this idea.
FOOD-BORNE INFECTIONS (FAECAL–ORAL TRANSMISSION)
Food-borne disease due to microbes can be split into two pathogenic mechanisms:
• intestinal infections,
• intoxications.
Intestinal infections cause diarrhoea following the multiplication of bacteria within the intestine,
whereas intoxications cause diarrhoea and/or vomiting after the ingestion of a toxin present in the
contaminated food. Intoxications occur because the organism has multiplied in the food and released
enterotoxins that are ingested (if they are not inactivated by cooking).
The mechanisms of staphylococcal and salmonella food poisoning illustrate how
preventing food poisoning can be achieved by preventing multiplication either in the food or in the
intestine. Complete elimination of the organism from the food is not necessary; instead, preventing the
organism from multiplying will prevent the required number for the infectious dose or producing toxin.
Note that viruses that cause food-borne disease will not be able to multiply in food or water but simply
utilise them as the vehicle for transmission.
One mechanism that attempts to maximize the opportunities for transmission is the carrier state. A carrier is a person who is passing an organism into the environment without showing any symptoms or
recognised pathology. Salmonella typhi is an organism that can infect people and maintain itself in the
gallbladder (bile duct) so that it is released in low numbers into the intestine. The person may or may not
have a symptomatic illness prior to becoming a carrier. ‘Typhoid Mary’ serves to illustrate the condition.
Mary Mallon lived and worked in the catering business, against the strict instructions from the New
York State that forbade her to handle food. One can imagine the confusion in her mind that an
apparently healthy woman was causing deaths through outbreaks of typhoid. Finally, imprisonment was
the only recourse left to the authorities to prevent further cases of typhoid. In general, the reasons for
why some people become carriers and others do not remains a mystery. With typhoid carriers, it is of
interest to note that gallstones are usually present and it is suggested that they predispose to carriage.
The transmission of microbes from host to host is the key parameter in the persistence of an obligate
human parasite within a community. What features help the efficiency of transmission?
Cited By Kamal Singh Khadka
Msc Microbiology, TU.
Assistant Professor In Pokhara Bigyan Tatha Prabidhi Campus(PBPC), Pokhara University, PNC, LA, NA.
Pokhara, Nepal.
SUGGESTED REFERENCES LINKS:





Comments